Para interpretar la semiología de los trastornos motores, es necesario conocer la jerarquía del control del sistema motor.
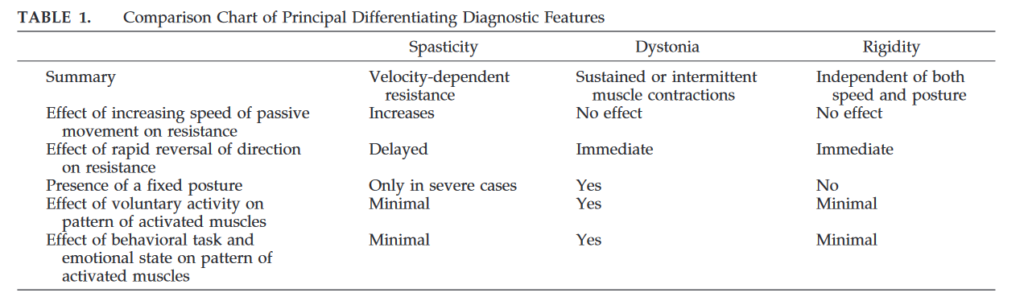
- Rigidez.
- Distonía.
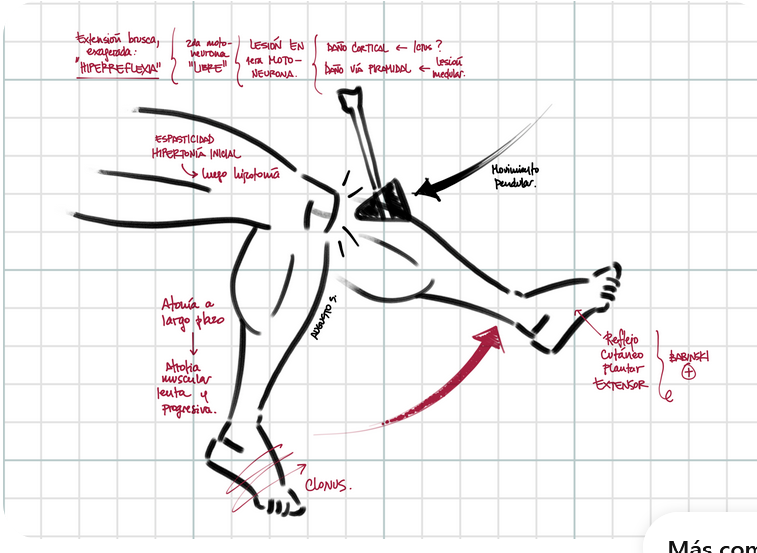
- Espasticidad.
Técnica de exploración.
For evaluating a hypertonic joint, the clinician should elicit the parents’ description of abnormal tone and involuntary movements, including whether movements occur with action or at rest, and whether there are particular trigger movements or task specificity. Observe posture at rest and the position of the limbs with respect to gravity. Observe the child lying, sitting, walking, and running, if possible. If complaints include abnormal performance or postures in response to specific activities or tasks, then the child should be observed while performing the affected task. Any abnormal fixed, twisted, or repetitive posture should be noted, as well as the degree of functional limitation.
The following observations should be performed for each joint to be tested. Recognizing the contribution of anxiety to tone, the child should be relaxed as much as possible during the examination and the body part being examined should be supported against gravity. The head should be maintained in the midline to avoid contributions to tone from the tonic neck reflex. In addition, if lying supine, then the head and trunk should be resting comfortably.
- Palpate the muscles to determine whether contraction occurs at rest.
- Measure resistance to movement of the affected joint with the child supine, seated, and standing, if possible, as well as while distracted.
- Measure passive range of motion at very slow (3 seconds to complete the movement), intermediate (0.5 second to complete the movement), and fast (as rapidly as possible) speeds. Note the resistance at the onset of movement, the presence or absence of a “catch” occurring at some time after the onset of movement, and the joint angle at which the catch occurs.
- Perform sudden reversal in the direction of movement at slow, intermediate, and fast speeds, and note the presence or absence of increased resistance immediately on reversal (suggesting co-contraction) or at some time after (suggesting a spastic catch), as well as any velocity dependence.
- Instruct the child to move the same joint on the contralateral side and observe for involuntary movement, then test for a change in resistance to slow, passive movement. Instruct the child to move a distant and unrelated joint (eg, by opening and closing 1 fist) on the contralateral side and then the ipsilateral side, and observe for involuntary movement or a change in resistance to passive movement.
Síntomas motores deficitarios.
- Debilidad (activación muscular insuficiente). Es importante diferenciar la debilidad muscular de la debilidad piramidal.
- Control motor selectivo reducido (inhabilidad para activar un patrón específico de músculos).
- Ataxia (inhabilidad para activar el patrón correcto de músculos durante el movimiento).
- Apraxia y dispraxia del desarrollo (inhabilidad para activar el patrón correcto de músculos para realizar una tarea, task-oriented).
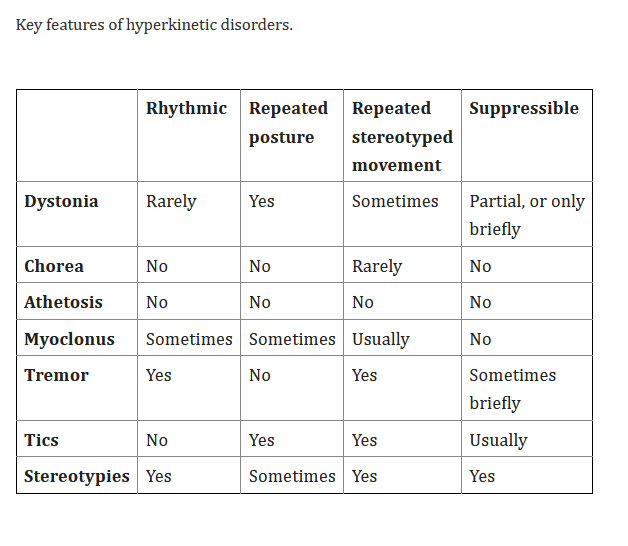
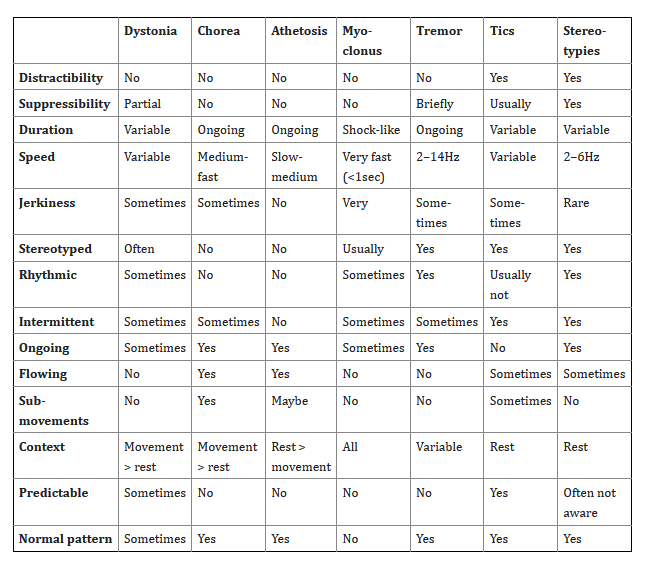
Trastornos hipercinéticos.
- Distonía.
- Corea.
- Atetosis.
- Mioclonus.
- Temblor.
- Tics.
- Estereotipias.
Trastornos hipocinéticos (parkinsonismo).
| Parkinsonism subtype | Definition according to 4 axes I. Age of onseta II. Clinical features III. Outcome IV. Etiology |
|---|---|
| Developmental parkinsonism | I. Infancy or early childhood II. Hypotonia, hypokinesia, bradykinesia, derangement of postural development, GDD, rest tremor or other coarse oscillatory jerks, periodic fluctuation of symptoms, dysautonomia, OGC, persistence of fetal motor patterns III. Persistent responsiveness to dopaminergic drugs and/or precursors of biogenic amines. Normal neurological development in early treated subjects, variable degrees of ID with or without MDs in late treated subjects, non-degenerative progression in untreated/late treated subjects IV. Primary Neurotransmitter disorders (e.g. TH, SR, AADC, PTPS deficiency) |
| Infantile and early childhood degenerative parkinsonism | I. Infancy or early childhood II. Severe rigid-hypokinetic syndrome, multifocal myoclonic jerks or coarse oscillatory jerks, dystonia, lack of postural development, progressive GDD, dysautonomia, OGC III. Initial dramatic response to dopaminergic drugs followed by response deterioration in WARS2 deficiency. No available treatment for DAT deficiency. Progressive course also documented by the remarkable alteration of DaTSCAN imaging IV. Primary or secondary Neurotransmitter disorders (e.g. DAT, WARS2 deficiency) |
| Parkinsonism in the setting of neurodevelopmental disorders | I. Childhood to adolescence II. Early-onset neurodevelopmental disorder (GDD, ID) followed by emergence of parkinsonian features over time. Epilepsy frequently associated III. No clear progression over time. Possible phases of regression followed by stabilization IV. Neurodevelopmental disorders (e.g. MECP2) |
| Parkinsonisms in the setting of multisystemic brain diseases | I. Childhood to adolescence II. Association with signs of multisystem brain involvement (spasticity, ataxia, myoclonus, dystonia, chorea, cognitive deterioration/dementia, epilepsy, etc.). Phenotype can be dominated by the other features associated with parkinsonism III. Progression over time associated with specific brain imaging abnormalities or metabolic alterations IV. Neurodegenerative or neurometabolic disorders with multisystem involvement (see Table 2, Table S1 for a list of conditions) |
| Juvenile parkinsonism and dystonia-parkinsonism | I. Childhood (rarely), adolescence II. Parkinsonism is the predominant manifestation, mainly in the form of atypical parkinsonism, with or without dystonia, myoclonus, and cognitive decline III. Levodopa response, onset of motor complications, and progression of parkinsonian signs can vary according to the specific genetic condition (e.g. good levodopa response in DNAJC6, SYNJ1, PINK1, no response in PRKRA, ATP1A3; early motor complications in Parkin and PINK1; slow progression in SYNJ1, rapid progression in DNAJC6) IV. Primary dystonia or monogenic parkinsonism genes (e.g. PRKRA, ATP1A3, Parkin, PINK1, SYNJ1, DNAJC12, DNAJC6) |
| Acquired parkinsonism | I. Infancy to adolescence II and III. Clinical features and outcome variable depending on etiology IV. Asphyxia, infections, immunomediated disorders, intoxications, drugs, tumors, hypoparathyroidism and pseudohypoparathyroidism, hydrocephalus (see Table 3, Table S2) |